A Hidden Battle Within the Body
Despite significant advancements, organ transplantation remains one of the most complex and challenging medical treatments, requiring deep knowledge of how the immune system interacts with transplanted organs. In general, by inhibiting T-cell activation pathways and reducing the production of harmful antibodies, transplant rejection can be prevented, and immunological tolerance can be strengthened. This approach is particularly important in critical stages of the immune response, including T-cell differentiation, function, and interactions with other immune cells.
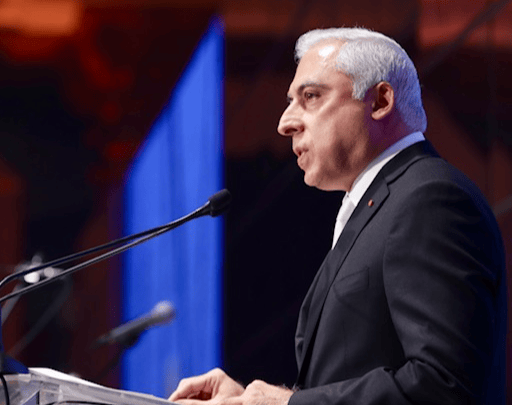
According to Mohamed Sayegh, the most fundamental question in this field is: “What are the mechanisms of immunological tolerance, and how can we trick the immune system into accepting a foreign organ without rejection and without immunosuppression?”
MSTF media reports:
Organ transplantation, one of the most advanced medical treatments, offers patients with organ failure a second chance at life, restoring the function of vital organs like heart, kidneys, liver, and lungs. Among these, kidney transplantation is the most common. In recent years, the number of transplants has increased, with significant advancements having been achieved in the field. Most transplants are allogeneic. This type uses transplants from someone other than the patient with similar genetic characteristics (except an identical twin). A major challenge in allogeneic transplantation is the immune system’s reaction to the new organ, which can lead to its rejection. To prevent this, patients have to continuously take immunosuppressive drugs, which help the body accept the new organ but weaken the immune system, and increase the risk of infections and complications such as high blood pressure and kidney damage.
The Immune System: Protector or Attacker?
The body’s immune system acts as an army, defending it against external entities such as viruses, bacteria, and even transplanted organs. When an organ from a donor is transferred to the recipient’s body, the immune system has to decide whether to accept it as a new part of the body or identify it as a threat. In most cases, the immune system naturally identifies the transplant as a danger, causing a reaction called transplant rejection. The rejection signifies that the body has identified the transplanted organ as foreign, and has started attacking it. Such an attack can seriously damage the organ, disrupt its function, and damage the recipient’s body.
The Secret of Recognition
The immune system employs several mechanisms to identify threats, one of the most important of which is using antigens. Antigens are special molecules that enable the immune system to identify threats. They are typically found on the surface of the major histocompatibility complex (MHC) molecules, which help the immune system distinguish between “self” and “non-self.” For example, if the host’s MHC molecules do not match those of the transplanted organ, the immune system gets alarmed and initiates a defensive response against it. The immune system’s reactions are highly complex, mostly caused by the recognition of molecular differences among various tissues. To put it succinctly, the greater the match between MHC molecules, the lower the chances of rejection, and the higher the chances of organ survival.
During the process of assessing compatibility, dendritic cells, known as the “messengers of the immune system,” collect antigens from the transplanted organ and send them to T-cells. This information transfer activates immune responses, ultimately leading to organ rejection. One of the leading scientists working to overcome challenges in organ transplantation is Mohamed Sayegh. Research in this area, particularly by Sayegh who is a prominent scientist in developing therapeutic strategies in the field, promises remarkable progress in medicine. To better understand his contributions, we must first take a step backwards to see how the immune response to the transplant is formed.
Unlocking Protection
One of the methods researchers use to prevent transplant rejection is to block the pathways that allow the immune system to initiate an attack on the transplanted organ. One such pathway, highlighted in the research of Mohamed Sayegh, is the CD28-B7 pathway (the interaction of B7 proteins on antigen-presenting cells with the CD28 molecule on immune cells), which plays a role in T-cell activation. When this pathway is blocked, T-cells can no longer become activated and attack the transplanted organ. Sayegh’s 1995 research findings showed that using the CTLA4Ig molecule can block this pathway, effectively reducing immune responses and preventing the immune system from attacking transplanted tissues.
Decoding the Missing Piece
Sayegh’s research contributed to the study of other T-cell stimulatory molecules, including members of the CD28 and B7 families. In 2003, he published a paper reporting the complex functions of a new T-cell stimulatory molecule, ICOS (Inducible Costimulator). The CD28 family includes multiple molecules, one of which is CD28 itself. Interestingly, ICOS is also a part of this family, but unlike CD28, which is permanently present on the surface of T-cells, ICOS appears only after T-cell activation and in response to specific stimuli. This makes ICOS a key molecule in the processes that help regulate immune responses.
Sayegh has shown that ICOS plays a crucial role in predicting transplant acceptance or rejection and influences how T-cells recognize transplant antigens. This recognition can occur directly—by detecting foreign antigens—or indirectly, after antigens are processed by the recipient’s “self” cells and presented to T-cells. Moreover, the interaction between ICOS and similar molecules on the surface of dendritic cells and other immune cells plays a vital role in regulating and boosting immune responses. Research has also shown that inhibiting ICOS during the early or late stages of transplantation can affect organ survival and acceptance.
Shutting Down the Attack
As mentioned earlier, after an organ transplant, T-cells can attack and reject the transplanted organ. Also, ICOS is a key molecule that strengthens immune responses. To study this pathway in detail, Sayegh’s research team conducted experiments using animal models, in which new hearts were transplanted into mice. They inhibited the ICOS pathway at two different time points. Early inhibition led to severe immune reactions and quick rejection, while late inhibition reduced inflammation and increased the chance of transplant acceptance.
When the ICOS pathway is blocked, T-cells can no longer interact effectively with dendritic cells. This has led recent findings to establish ICOS as a promising therapeutic target, thus enabling the development of new drugs that reduce immune responses through inhibiting this pathway. During clinical trials, these drugs have prevented inflammation in transplanted tissues and reduced the risk of rejection.
From Tissue Compatibility to Transplant Success
The major histocompatibility complex (MHC) in humans is known as the human leukocyte antigen (HLA). HLA testing is one of the most important tools that enables doctors to increase the chances of transplant success. By analyzing tissue compatibility between donor and recipient through MHC molecule identification, these tests help predict whether the recipient’s immune system will reject the transplanted organ or accept it. The more precise the match, the lower the risk of rejection and the greater the chances of transplant survival.
One of the major challenges in organ transplantation is that each person’s immune system reacts differently to transplanted organs due to genetic differences. Some individuals’ immune systems may easily accept the transplanted organ, recognizing it as part of the body, while others may quickly reject it as a threat and start an immune attack. Therefore, advanced and precise testing is essential before transplantation to assess tissue compatibility.
"This material was originally published in the second issue of the International Observatory Journal."